How Can Gastroparesis Affect You
Nausea is common and may be associated with vomiting. Bloating, abdominal pain, and weight loss, are also common. In diabetic and idiopathic gastroparesis the symptoms can be heartburn with bloating, feeling full soon after starting a meal, nausea/vomiting and regurgitation of food are also common. Pain is more frequently experienced with people diagnosed with idiopathic gastroparesis. You may feel full very quickly during eating and be unable to finish eating a normal size meal, but symptoms can also occur in-between meals and symptoms occurring during the night have also been reported. Usually symptoms occur in combination and not in isolation.
Children commonly experience symptoms of vomiting, abdominal pain, weight loss, feeling full soon after starting a meal and feeling very full after eating a normal sized meal.
Weight loss can occur, so supporting your nutrition is essential to try and prevent further weight loss. Severe symptoms that result in dehydration and severe malnutrition may require hospitalisation for treatment.
You may feel that you have a food intolerance, but this is not usually the case. As symptoms are caused by the physical action of slow stomach emptying and not by food intolerance, elimination diets do not generally help with gastroparesis and should be avoided as they can lead to malnutrition. See below for dietary advice which may be helpful.
What Are The Symptoms Of Gastroparesis And Gastric Motility Disorders
Symptoms include bloating, pain or swelling in the abdomen , nausea, and vomiting. People feel full after eating just a few bites and may have no appetite. Anorexia, heartburn, gastroesophageal reflux, and abnormal blood sugar levels may occur. People can lose weight because they dont get enough nutrients.
Gastroparesis Treatment & Diet
There is no cure for gastroparesis, but medication and diet changes can help in most cases. In very severe cases, surgery may be recommended.
Treatment usually begins by identifying and treating the underlying cause of gastroparesis. If the cause is diabetes, your doctor will make recommendations for treatment.
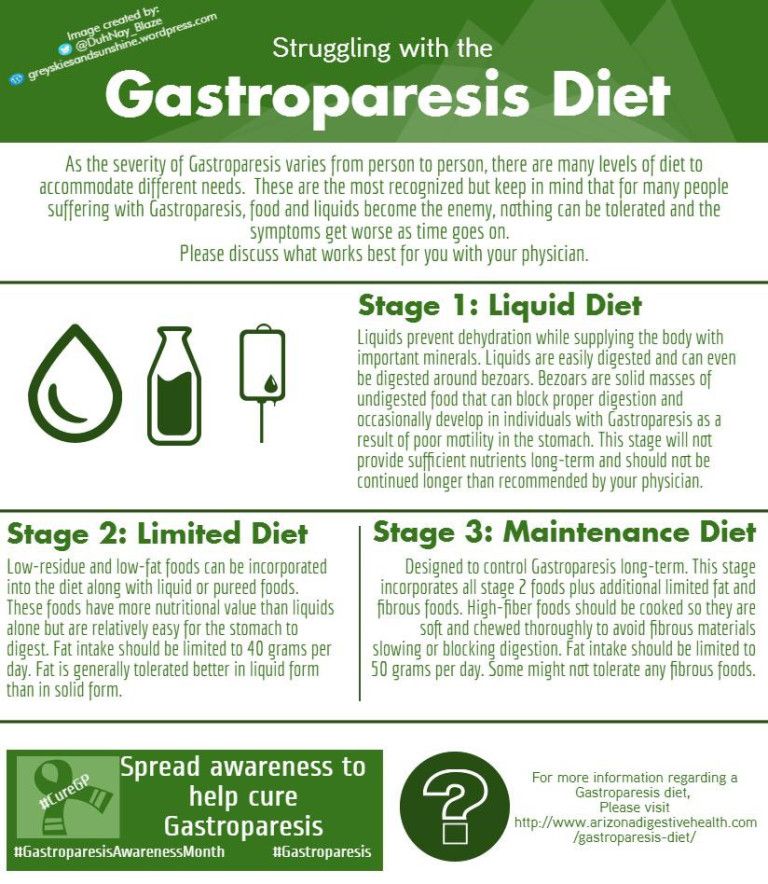
Gastroparesis Diet
Making sure you get adequate nutrition is important when managing gastroparesis. Diet changes usually help people manage gastroparesis and are the first step in treatment. It may be helpful to visit with a registered dietitian who can work with you to identify foods that are easier to digest.
Most people can lead a relatively normal life by eating softer foods and drinking supplemental nutritional drinks to ensure they get the calories and nutrients they need.
Other gastroparesis diet advice includes:
- Eat smaller meals
- Chew food completely
- Choose cooked vegetables and fruits over raw, uncooked fruits and vegetables
- Avoid high-fiber vegetables and fruits, like broccoli and oranges
- Avoid fatty foods
- Puree your food or eat soups if liquids are easiest to swallow
- Drink plenty of water each day
- Take a walk after you eat
- Avoid alcohol, smoking, and carbonated beverages
- Try not to lay down within 2 hours of eating
- Take a daily multivitamin
Below are recommended diet choices for people with gastroparesis. This is not an exhaustive list, and a dietitian can provide a more complete list.
Read Also: What Could Cause Your Stomach To Hurt
Causes And Risk Factors
There are several risk factors that are considered to play a role in the conditions cause, such as vagus-nerve damage. The vagus nerve is the longest cranial nerve in the body and is responsible for many functions. It is especially essential for proper operation of the digestive tract. If the vagus nerve is damaged, transfer of food from the abdomen to the small intestine is reduced because the muscles will not operate properly.4
Type 1 and type 2 diabetes are known to damage the vagus nerve. Some autoimmune diseases and virus infections are also believed to have a negative impact on the vagus nerve. In certain cases, the vagus nerve stops working properly due to drinking excessive alcohol. Surgical complications could also affect the vagus nerve.4
Other factors that can increase the risk of gastroparesis include abdominal or esophageal surgery, infection , certain medications that slow the rate of stomach emptying , nervous system diseases and hypothyroidism.4 Complications resulting from gastroparesis are shown in TABLE 1.
Sometimes, treating the cause may stop the problem. If diabetes is causing gastroparesis, patients must control their blood glucose levels. Acute hyperglycemia may impair gastric motor function as well as inhibit the action of prokinetic drugs, such as erythromycin. In patients with type 1 diabetes, gastroparesis can be an indication for insulin-pump therapy.5
Should I Change My Diet If I Have Gastroparesis
One of the best ways to help manage the symptoms of gastroparesis is to change your daily eating habits. For instance, instead of three meals a day, you can eat six small meals. In this way, there is less food in your stomach you wont feel as full, and it’ll be easier for the food to leave your stomach.
Another important factor is the texture of food. Your provider may recommend liquids and low residue foods .
You should also avoid foods that are high in fat and fiber .
- The National Institute of Diabetes and Digestive and Kidney Diseases. Gastroparesis. Accessed 7/23/2018.
- American College of Gastroenterology. Gastroparesis. Accessed 7/23/2018.
- Society of American Gastrointestinal and Endoscopic Surgeons. Early human experience with Per-Oral Endoscopic Pyloromyotomy . Accessed 7/23/2018.
- Landreneau, J.P., Strong, A.T., El-Hayek, K. et al. Laparoscopic pyloroplasty versus endoscopic per-oral pyloromyotomy for the treatment of gastroparesis. Surg Endosc . https://doi.org/10.1007/s00464-018-6342-6
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.Policy
Don’t Miss: How To Heal Stomach Pain
When Should I Seek A Doctors Help
You should seek a doctors help right away if you have any of the following signs or symptoms:
- severe pain or cramping in your abdomen
- red blood in your vomit, or vomit that looks like coffee grounds
- sudden, sharp stomach pain that doesnt go away
- vomiting for more than an hour
- feeling extremely weak or fainting
- difficulty breathing
You should seek a doctors help if you have any signs or symptoms of dehydration, which may include
- extreme thirst and dry mouth
- urinating less than usual
- dark-colored urine
- sunken eyes or cheeks
- light-headedness or fainting
You should seek a doctors help if you have any signs or symptoms of malnutrition, which may include
- feeling tired or weak all the time
- losing weight without trying
- abnormal paleness of the skin
How Is Gastroparesis Managed
Although gastroparesis cannot be cured, the symptoms can be relieved. You can ease symptoms by:
- eating fewer, smaller meals
- eating easy-to-digest foods
- taking medicines to improve the muscles around the stomach contraction and control nausea
If things dont improve with changes to diet the and medicine, you can have a pacemaker inserted in the stomach to stimulate the muscles in the stomach. This is called gastric electrical stimulation. Talk to your doctor.
If you have diabetes, irregular emptying of the stomach can make it difficult to control blood glucose levels. It is important to get advice from your doctor.
Very severe cases may be treated by injecting botox into the valve between the stomach and small intestine, inserting a feeding tube, or surgery.
Read Also: What Causes Swollen Stomach And Pain
Its Often Overlooked And Can Lead To Bloating Abdominal Pain And Other Troubles
When you eat a meal, you probably dont think about the amount of time it takes your body to digest the food. But for many people, this is the key to uncovering a host of digestive illsand even some seemingly unrelated concerns such as chronic fatigue.
WHEN FOOD MOVES TOO SLOWLY
In healthy adults, digestion time varies, but it generally takes about four hours for a meal to leave the stomach before passing on to the small intestine and colon.
What happens: When food enters the stomach, signals from hormones and nerve cells trigger stomach acid, digestive enzymes and wavelike peristaltic contractions of the muscles in the stomach wall. Together, they break down the meal into a soupy mixture called chyme, which peristalsis then pushes into the small intestine.
This process is known as gastric motility. And when gastric motility is impededwhen stomach emptying slows to a crawl, even though nothing is blocking the stomach outletits called gastroparesis.
Surprising fact: An estimated one out of every 55 Americans suffers from gastroparesisbut the condition is diagnosed in only one out of every 90 people who have it.
GETTING THE RIGHT DIAGNOSIS
If youre experiencing the symptoms of gastroparesis, see your primary care physician. He/she may refer you to a gastroenterologist. Its likely the specialist will order the gold standard for diagnosing gastroparesis, a test called gastric emptying scintigraphy.
FINDING THE CAUSE
GETTING THE BEST MEDICAL CARE
ALTERNATIVE THERAPIES
Botulinum Toxin Type A
Botulinum toxin type A is a toxin that reduces muscle activity. Its been studied in gastroparesis and other gastrointestinal tract disorders.
Injection of the medication into the pyloric sphincter muscle improved this condition in some studies. However, due to contradictory results and the small size of most studies, scientists that more research is needed before it can be recommended.
Recommended Reading: Can Asthma Cause Stomach Pain
Upper Gastrointestinal Barium Contrast Radiography
Barium contrast radiography is an X-ray study. It is a commonly used procedure to diagnose gastroparesis.
During barium contrast radiography:
- You swallow a contrast solution called barium.
- The barium coats your esophagus and gastrointestinal tract, making it easier for the doctor to detect abnormalities.
- An X-ray is taken.
- Your doctor can determine if there are delays in the liquid emptying from your stomach.
Delayed Gastric Emptying Causes Symptoms And Treatment
by Adam Smith | Feb 10, 2022 | Healthy Lifestyle, Vaccine and Cure
Stomach disorders come in a wide range. One of the most common ones is delayed gastric emptying, which is a condition that affects both adults and children. The disorder, which experts also refer to as gastroparesis, typically occurs when your stomach takes more time than it should empty food to the small intestines.
If you suspect that you have delayed gastric emptying, what are the things you need to consider? Read further to learn more about the causes, symptoms, and the best treatment for you.
Don’t Miss: How To Work On Stomach Fat
Gastroparesis: Understanding Slow Stomach Emptying And Finding The Solution For You
Feeling full or uncomfortable after eating is perfectly normal from time to time. But if youre noticing abdominal pain and bloating are becoming a frequent occurrence after a meal especially along with other symptoms like nausea, vomiting, acid reflux, regurgitating undigested food and unintentional weight loss these may be signs of a serious condition known as gastroparesis.
Gastroparesis is a disorder characterized by delayed gastric emptying. The muscles that contract to help food move through the stomach and into your small intestine may be significantly slowed or even stop. It can feel as though theres a traffic jam in your gastrointestinal tract, even though theres nothing truly blocking your digestion.
What Are The Complications Of Gastroparesis
If food lingers too long in the stomach, it can cause bacterial overgrowth from the fermentation of food. Also, the food can harden into solid masses called bezoars that may cause nausea, vomiting, and obstruction in the stomach. Bezoars can be dangerous if they block the passage of food into the small intestine.
Gastroparesis can make diabetes worse by making blood glucose control more difficult. When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels rise. Since gastroparesis makes stomach emptying unpredictable, a persons blood glucose levels can be erratic and difficult to control.
Recommended Reading: How To Get Rid Of Stomach Pain And Bloating
Electrical Stimulation For Gastroparesis
One area of medical research is looking at electrical stimulation to treat gastroparesis. Small electronics are attached to the stomach wall. Once activated, they can cause the stomach to contract. Studies havenât shown significant improvements in stomach emptying, but have shown to reduce bothersome symptoms like nausea and vomiting.
A New Approach To Managing Gastroparesis
Manouchehr Saljoughian, PharmD, PhDAlta Bates Summit Medical CenterBerkeley, California
US Pharm. 2019 44:32-34.
Gastroparesis is a chronic disorder that affects a significant subset of the population. Ordinarily, strong muscular contractions move food through the digestive tract. In gastroparesis, this mechanism is disrupted, and undigested food stays in the abdomen for a long time and makes a person feel nauseous with the urge to vomit. Gastroparesis can also cause a lack of appetite, which may lead to malnutrition, and patients who are not eating can expect discomfort, bloating, and heartburn.1
The pathophysiology behind gastroparesis is varied and depends on disease etiology. Vagal and/or autonomic neuropathy play an important role in the development of diabetic gastroparesis, and it is estimated to occur in up to 20% to 40% of patients with diabetes. Gastroparesis can cause problems with blood sugar levels and nutrition. Sometimes, it is a complication of diabetes, and some people may develop gastroparesis after surgery. Although there is no cure for gastroparesis, changes to the diet, along with medication, can offer some relief.1,2
Recommended Reading: What Kind Of Doctor Specializes In Stomach Problems
How Should I Handle A Flare
Making changes to your diet and lifestyle is an effective way to manage symptoms of gastroparesis.
Eating several smaller meals per day, foods that are hard to digest, and swapping solid foods for liquid or pureed ingredients can all be beneficial.
Your doctor may also prescribe medications to help control symptoms like nausea or vomiting during a flare-up.
How Are Gastroparesis And Gastric Motility Disorders Diagnosed
For diagnosis, the health care provider may use a nuclear medicine test called a gastric emptying test . The test involves eating foods or drinking liquids containing a radioactive substance. The dose isnt dangerous. A device similar to a Geiger counter tells how fast food leaves the stomach. The health care provider will also perform a physical exam and obtain a detailed medical history to rule out other causes . The health care provider may also order breath tests, ultrasonography, upper endoscopy, computed tomography, manometry, and X-rays.
Read Also: Is It Bad For Babies To Sleep On Their Stomach
What To Ask Your Doctor:
- Are there any medications that can cause these symptoms and if so, what alternatives can I try?
- What treatments are available to my situation and what are the benefits and drawbacks of them?
- Can I be referred to a dietitian to help me with my diet?
- Can I see a diabetes specialist to help me with my diabetes control?
- Can I talk to someone about my feelings at having to manage my symptoms?
When To Seek Medical Advice
See a GP if you’re experiencing symptoms of gastroparesis, as it can lead to some potentially serious complications.
These complications include:
- dehydration from repeated vomiting
- gastro-oesophageal reflux disease where stomach acid leaks out of your stomach and into your food pipe
- malnutrition when your body is not getting enough nutrients
- unpredictable blood sugar levels this is a particular risk in people with diabetes
Don’t Miss: Does Your Stomach Hurt If You Are Pregnant
What Are Gastroparesis And Gastric Motility Disorders
The stomach grinds food into small pieces and sends them to the small intestine. Gastric motility disorders include delayed gastric emptying , rapid gastric emptying , functional dyspepsia , and cyclic vomiting syndrome.
In gastroparesis, the stomach doesnt work well. It doesnt contract, crush food, or send food to the small intestine in a normal way. Food stays in the stomach too long. Digestion isnt normal. Food can harden into solid chunks that may cause nausea and vomiting and block the stomach.
Gastroparesis affects males and females of almost any age.
Are There Any Risks To The Test

You should not have a gastric emptying study or an upper GI series if you are pregnant or think you may be pregnant. Radiation from these imaging tests can be harmful to an unborn baby. For others, there is little risk to having an imaging test. The dose of radiation is very low and not considered harmful for most people. But talk to your provider about all the x-rays you’ve had in the past. The risks from radiation exposure may be linked to the number of x-ray treatments you’ve had over time.
There is very little risk to having a gastric breath test or taking a smart pill. In rare cases, a smart pill may get stuck in the digestive system. If the pill takes longer than several days to leave your body in a bowel movement, contact your health provider.
Recommended Reading: How To Control Gas Problem In Stomach
Measurement Of Gastric Emptying
Gastric emptying scintigraphy is considered the standard method for measurement of gastric emptying, providing physiologic, noninvasive, quantitative measurement of gastric emptying.11 GES involves ingestion of a radiolabeled meal followed by serial measurement of radioactivity in the stomach, which directly correlates with the volume of meal remaining in the stomach.12 An example is shown in Fig. 28.2. Variation in the test protocols used to perform GES is a significant limitation of this technique, and attempts to standardize the methodology of GES in adults have been made.11 GES is performed after a period of fasting. Medications that can affect gastric emptying, including prokinetic medications and opiates, should be discontinued prior to the test. The duration of discontinuation should be based on the medications half-life, but for most medications 48 to 72 hours should suffice. Serotonin receptor antagonists like ondansetron should have little effect on gastric emptying and can be given prior to GES. For children with diabetes, it is important to recognize that hyperglycemia delays gastric emptying.11
Chen Sheng Low, … Mohamed El-Sayed, in, 2022
What Are The Symptoms Of Gastroparesis
Nausea and vomiting are two of the most common symptoms of gastroparesis, most likely stemming from the sluggish emptying of the stomach. Typically, these symptoms occur toward the end of meals or soon after meals are finished. A third common symptom is abdominal pain caused by a combination of motor nerve and sensory nerve dysfunction. When motor nerves arent working properly, food and liquid can be detained in the stomach. When sensory nerves arent working well, signals between the gut and the brain are not communicated effectively, which can cause pain, nausea, and vomiting.
A growing body of evidence suggests that gastroparesis overlaps with a disorder of gut-brain interaction called functional dyspepsia, which is recurring indigestion that has no apparent cause. Other health problems can cause similar symptoms as gastroparesis, such as gastric outlet obstruction and cyclic vomiting syndrome, or even conditions beyond the gut, such as glandular disorders. So its important to discuss any symptoms that are bothering you with your doctor to get the correct diagnosis.
Recommended Reading: Why Is My Stomach So Swollen