After Gastric Sleeve Surgery Costs
There are not many costs after gastric sleeve surgery. Unlike the Lap Band, you will not need regular adjustments from your surgeon to ensure the proper tightness. Below are a few important points to keep in mind.
- Nutritionist appointments are often out of pocket or negotiated before surgery. These can range from $50 USD per visit to over $100 per visit.
- Compared to gastric bands, there is very little required follow-up with gastric sleeves and therefore lower costs.
- Post-surgery follow-up visits with your bariatric surgeon are typically free.
- Complications can be extremely expensive. If the surgery is covered by insurance, then complications are typically covered as well. Treatment of wound site infections is typically paid for by the hospital or surgery center.
How Does Medicare Regard Weight Loss Surgery
Unlike cosmetic surgery, Medicare considers weight loss surgery as a genuine health intervention.
Every surgical procedure that is supported by Medicare is listed in a large directory called the MBS and each has its own unique Item Number.
Weight Loss Surgery is no different, the Item Numbers for are Gastric Bypass and Mini Gastric bypass is 31572 and for Sleeve Gastrectomy it is 31575. This means that Medicare will partially cover the costs involved in your surgery.
What Weight Loss Surgery Is Covered By Insurance
The answer varies from insurer to insurer, so its important to ask all the pertinent questions before making a decision regarding surgery.
Most health insurance policies will not cover bariatric surgery.
Bariatric surgery is a type of serious weight loss surgery used to treat severe obesity and other health problems resulting from being overweight.
Bariatric surgery is sometimes covered under special circumstances, such as when the patient has hernia complications and the procedure can be performed to correct the problem.
Sometimes the health fund will cover it if the patient undergoes extreme psychological stress after having bariatric surgery and it can be proven to be medically necessary.
If youre unsure whether your surgery is covered by your health fund, check with your health insurer.
What weight-loss surgery is covered by insurance companies?
Generally, surgery is not covered by most health insurance plans, even though weight-loss surgery is very effective in treating most overweight patients.
Some insurance companies will cover bariatric surgery if its performed by qualified doctors and its performed for a life-threatening condition.
Ask your doctor or health fund provider whether your surgery is considered a life-threatening condition.
If your insurance company covers bariatric surgery, most health funds will not cover it, because its considered elective surgery.
Also Check: How To Lose Internal Stomach Fat
How Does A Lap Band Work
The LAP-BAND system is a weight loss tool that can be used to help patients achieve their weight loss goals. The minimally invasive surgical procedure is usually performed laparoscopically in a surgical center. The procedure involves placing an adjustable gastric band around the upper portion of the stomach. The band can then be tightened limiting the amount of food needed to feel full. Through healthy portion control, good nutrition and other healthy lifestyle choices patients are able to lose excess weight and keep it off. The LAP-BAND procedure is a safe, minimally invasive solution that helps patients lose weight gradually while improving their overall health. Below we dive into the cost of LAP-BAND surgery, if insurance covers the procedure and how LAP-BAND financing can help.
Saving Money After Surgery
Its important to note that youll also save money after you lose weight. And it adds up. Not only is your diet considerably restricted after gastric bypass surgery, but medical bills, prescription co-pays, labs, and food bills will decrease. Use our affordability calculator to see how much youll save 3 years after surgery.
You May Like: What Can I Take To Stop My Stomach From Hurting
Weight Loss Surgery And Insurance Coverage
According to The American Society for Metabolic & Bariatric Surgery , the average cost for bariatric surgery runs anywhere between $17.000 and $26,000 but the exact cost will be dependent on the type of surgery you have, your overall health, and current BMI, and if you encounter any complications, etc.
There is much evidence to support that the cost of surgery is much less than treating the associated obesity-related conditions long-term. Most insurance companies will cover gastric sleeve surgery but not the less expensive non-surgical options such as a gastric balloon or endoscopic sleeve gastroplasty.
Endoscopic sleeve gastroplasty has a proven track record of delivering results comparable to gastric sleeve surgery. It does not require surgery, it is less expensive, has fewer complications, and offers a faster recovery. This FDA-approved weight loss procedure is gaining popularity and has proven to result in significant weight loss.
Even with the supporting evidence and FDA approval, insurance companies do not yet cover non-surgical EGS and currently only cover expensive surgery. Insurance companies in general are slow to cover new procedures, but most bariatric surgeons feel that endoscopic sleeve gastroplasty will be covered by insurance companies in the future because it would benefit all parties.
All You Need to Know About Endoscopic Sleeve Gastroplasty – Accordion Procedure – Endosleeve
Not All Policies Are The Same
The first thing to understand is that every insurance policy is different. You might have health insurance that covers weight loss surgery, at least in part, and you might not.
Since the passing of the Affordable Care Act, all medical insurance policies sold on the Marketplace must offer obesity coverage. However, the ACA does not outline what this means. Insurance policies can decide that obesity coverage is strictly nutritional guidance or therapy sessions. Others might include certain medications. And others still can extend this coverage to bariatric surgeries.
With that said, most companies offer at least partial coverage of gastric bypass, gastric sleeve, and lap band surgeries. If you are wondering, does Medicaid cover weight loss surgery? The answer is yes. However, there are limits for it and private policies.
Recommended Reading: What To Do To Ease Stomach Pain
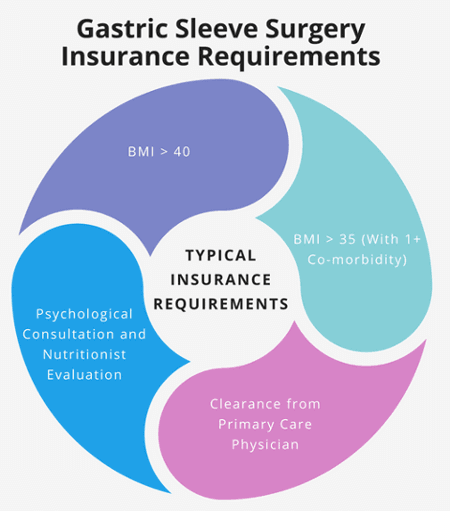
Requirements For Bariatric Surgery Coverage
Most insurance policies will require you to meet specific criteria before you are eligible for coverage. Each provider sets their own terms for this, so be sure to contact your insurance company and ask them about what requirements you must meet to qualify.
In most cases, you will need to meet some or all of the following for insurance policies to cover some or all of your surgery and related expenses:
- Be over the age of 18.
- Been overweight or obese for a certain number of years.
- Have a current BMI of 40+ or a BMI of 35+ with a comorbidity.
- Been diagnosed by a medical professional with morbid obesity.
- Be psychologically stable enough to undergo surgery and make the associated lifestyle changes.
Located in the Mesilla Valley of southern New Mexico between the stunning Organ Mountains and the rambling Rio Grande Memorial Weight Loss Center serves the 300,000 residents of Las Cruces New Mexico and Doña Ana County by performing bariatric procedures including Gastric Bypass surgery, Gastric Sleeve surgery and LAP-Band surgery. We offer the latest minimally invasive laparoscopic weight loss procedures available in the nation today. Our comprehensive weight loss surgery procedures include comprehensive pre-operative and post-operative care for our patients. Our weight loss surgery clinic in Las Cruces New Mexico provides the latest in diagnostic, therapeutic and rehabilitative services , all for the inpatient and outpatient.
Cigna Bariatric Surgery Requirements
In order to qualify for the Cigna weight loss surgery, you will need to meet the following Cigna bariatric surgery requirements 2019:
- You must be 18 years of age or older.
- You must have a BMI of more than 40 for at least the past 2 years.
- You must have a BMI of 35-39.9 for at least the past 2 years, and you must have at least one obesity-related illness.
- You must have participated in a medically-supervised weight loss program within the last 2 years.
- Your doctor must deem the bariatric surgery a medical necessity for you.
- You must have a psychological evaluation that shows you are capable of changing your lifestyle for weight loss.
YOU MIGHT WANT TO READ: Do I qualify for weight loss surgery?
Also Check: Does Menopause Cause Stomach Bloating
How Long Does It Take Bcbs To Approve Bariatric Surgery
Blue Cross Blue Shield will take up to 30 days on average to approve your request for bariatric surgery. Therefore, when you are planning to undergo a weight loss surgery with insurance coverage, plan ahead of time, and keep track of the time it takes to complete the BCBS approval process.
- Expedite the approval: To begin with, choose a hospital or bariatric surgeon that will help you meet the BCBS approval conditions quickly, and will follow up with them on your behalf. Prepare all the necessary documentation that BCBS may demand, such as health records, medical tests, diet and exercise report, and behavior modification class certificate .
- BCBS appeal process: If Blue Cross Blue Shield does not approve your pre-authorization for bariatric surgery, you will still have an option to file an appeal. With guidance from your surgeon, be prepared to counter each argument they have made to deny your coverage request. Follow the precise rules of the BCBS appeal process, and make your appeal within the stipulated time.
- Affordable surgery options: In a situation where you fail to get approved for bariatric surgery from BCBS and your appeal is also rejected, it still does not mean that you should deny yourself good health and a long life. Explore low cost bariatric surgery options, such as medical tourism with a trusted service provider. This will enable you to eliminate obesity and reclaim your health within your budget.
Does Insurance Cover Weight Loss Surgery
Weight loss surgery is a serious undertaking physically, emotionally, and financially. Without health insurance, bariatric surgery is financially inaccessible for many people, a sad fact because weight loss surgery is often a medical necessity.
For some, weight loss surgery is the last hope the final road to freedom from health complications. Dr. Robert Snow, bariatric surgeon at Snow Bariatric Center in Fort Worth and Flower Mound, Texas, has seen the pure joy that comes with being free from those constraints, and he wants weight loss to be as accessible as possible.
To navigate the beginning stages of weight loss surgery, its helpful to understand how and if insurance companies pitch in financially.
You May Like: How To Lose Stomach Fat Naturally
Medicare Requirements For Bariatric Surgery
Their criteria are similar to other insurance companies so if you want to know how to get weight loss surgery approved by Medicare, you must meet the following Medicare requirements for bariatric surgery:
- You must have a BMI of more than 35.
- You must have at least one obesity-related health problem
- You must have struggled with obesity for the last 5 years.
- You must have legitimate medical documents and health records from those last 5 years.
If you meet all these criteria, Medicare will need you to go through a lengthy process to receive their approval. This Medicare bariatric surgery approval process includes:
- Having a record of at least 1 attempt at a weight loss program under the supervision of a doctor.
- Showing proof that you failed at least 1 supervised weight loss program
- Undergoing blood tests for Pituitary, Adrenal, and Thyroid.
- Undergoing a full psychological evaluation.
Before You Get Weight Loss Surgery It Is Always Best To:
- Talk to your doctor about all of your options
- Clarify with the hospital or facility conducting your procedure how much you might pay for the surgery and aftercare
- Be aware of how much you may owe on your deductible, as this amount needs to be satisfied before Medicare can start to pay
- Know that copayments may still apply for the care you receive
Note: This material is provided for informational use only and should not be construed as medical advice or in place of consulting a licensed medical professional. You should consult your doctor to determine what is best for you.
Explore Medicare
Recommended Reading: Is Purple Mattress Good For Stomach Sleepers
Healthfirst Requirements For Gastric Sleeve
Once you have made sure that you are covered, you will need to meet the following HealthFirst requirements for gastric sleeve or any other bariatric surgery:
- You must be 18 years of age or older.
- Your BMI must be 40 or higher.
- Your BMI must be 30-39, and you must also suffer from an obesity-related illness including severe sleep apnea, diabetes, or a cardiovascular disease.
- You must have no untreated metabolic condition that may be causing your obesity.
- You must have been overweight for 2-5 years.
- You must show proof that youve tried losing weight through non-surgical methods.
- You must be able to pass a psychological evaluation showing that you are capable of making long-term changes to your diet and lifestyle.
Whats The Stomach Stapling Recovery Process Like
Most bariatric surgeries today are minimally invasive procedures that are performed laparoscopically.
Instead of the large incision needed for open surgery, youll only need a few small incisions in your abdomen. This speeds up your recovery.
After stomach stapling surgery, patients are usually in the hospital for 1 to 3 days. Once at home, youre encouraged to rest and to limit daily activities. It may take between 1 to 3 weeks to return to work.
About 1 month after surgery, you can slowly begin an exercise program to help increase weight loss.
Most people who have stomach stapling surgery feel tired and dont have much energy the first 2 weeks after the surgery. This is mostly due to the low calorie liquid diet thats needed after the surgery. This gets better once soft foods are introduced to the diet.
It takes about 6 weeks to fully recover from stomach stapling surgery and to get back to a normal daily routine. By then, most patients have already lost a noticeable amount of weight.
Also Check: How To Get Rid Of Deep Stomach Fat
How Long Does It Take Medicaid To Approve Weight
Medicaid also allows weight-loss surgeries if you meet criteria, but recent studies show approval make take longer.
Insurers usually take a month to approve weight-loss surgeries. However, wait times for Medicaid approval can take five months or more. During that time, Medicaid will review your records and input from your doctor before making the decision.
Does Insurance Cover Panniculectomy
In most cases, insurance companies do cover at least part of this procedure, but there are some policies that cover only a portion of the procedure.
This is why it is important to read the fine print of any policy you sign.
It is also important to keep in mind that many insurance companies require written documentation for this particular procedure.
This procedure is done on those who have undergone surgery for some kind of health problem.
And this surgery also has the added benefit of improving the patients general well-being as it reduces the risks of developing other health problems in the future.
According to experts on health insurance, this particular procedure is not considered necessary due to the fact that there are many surgical procedures available today that can achieve the same results as the surgery which was earlier performed on the patient.
However, most insurance companies will pay for this procedure if they see that the patient needs it for his or her own good.
This is because it is proven that the excess skin or tissue causing health problems may be removed surgically.
In many cases, the excess skin or tissue may cause breathing problems, heart problems, and other similar diseases, and hence the insurance company may pay for this procedure.
Why is Panniculectomy covered by insurance?
This procedure is usually covered by health insurance companies when the doctor states that it will help improve the quality of life for the patient.
Recommended Reading: How To Heal An Inflamed Stomach
Need To Convince Your Spouse
LAP BAND SURGERY COSTS
Paying cash for Lap Band surgery is expensive and you might need to convince your spouse or family members that its worth it. Yes, youll lose weight, feel better and reduce your long-term medical expenses. But will those savings actually offset the $10k cost of the procedure?
This calculator will show your expected savings over a 3 year period. Guess what? Your savings will likely offset the cost of Lap Band surgery within 3 years. Print your results or email them to your family or spouse.
Bariatric Surgery Improves Overall Health
The benefits of bariatric surgery have been the subject of much research and have been published through many different outlets. Many patients experience total remission of type 2 diabetes after losing weight as a result of bariatric surgery. Other weight-related illnesses and risks that are reduced after weight loss surgery are:
- Heart disease and stroke
- Urinary incontinence/bladder issues.
Recommended Reading: What To Use To Flatten Your Stomach
Experimental And Investigational Bariatric Surgical Procedures
Aetna considers each of the following procedures experimental and investigational because the peer-reviewed medical literature shows them to be either unsafe or inadequately studied: