Radionuclide Gastric Emptying Test
Radioscintigraphy measurement of the gastric emptying rate remains the gold standard for quantitative assessment of the emptying function of the stomach. To perform this test, patients are administered a standarised meal in which one component has been labelled with a radioisotopic -emitting marker. An external -camera quantifies the radioactivity in the area of the stomach in sequential images over 4 h. The rate of disappearance of the radioisotope corresponds to the gastric emptying rate . Solids and liquids are emptied from the stomach at different rates and can be independently evaluated by labelling each component with a different radioisotope .
What Is Diabetic Ketoacidosis
Diabetic ketoacidosis happens when your blood sugar is higher than normal and your insulin level is lower than normal. This imbalance in the body causes a build-up of ketones. Ketones are toxic. If DKA isnt treated, it can lead to diabetic coma and even death.
DKA mainly affects people who have type 1 diabetes. But it can also happen with other types of diabetes, including type 2 diabetes and gestational diabetes .
What Are The Complications Of Diabetic Gastroparesis
Sometimes, even with treatment, problems can happen that can upset how well you are managing your condition.
In addition to those that might happen with diabetes, diabetic gastroparesis can cause:
- Severe dehydration or loss of water and electrolytes from vomiting that does not stop.
- Esophagitis, pain and irritation in the esophagus .
- Bezoar , which can cause nausea, vomiting, or a blockage, or stop the body from using some medicines right away.
- Malnutrition, which happens when the body does not get the vitamins, minerals, or nutrients it needs. This can lead to weight loss and raise the risk for infection.
- Worsening quality of life from not being able to do what you want to do because of your symptoms.
Don’t Miss: What Causes Fluid In Your Stomach
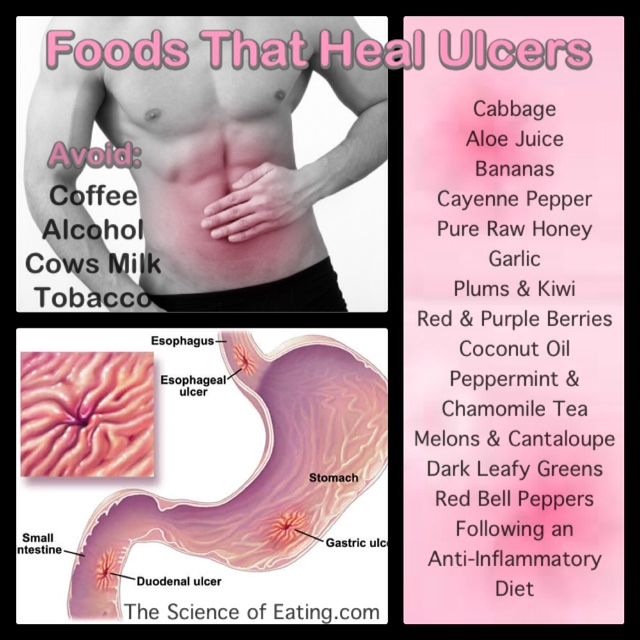
What Causes Stomach Ulcers
Your stomach normally produces acid to help with the digestion of food and to kill germs . This acid is corrosive, so some cells on the inside lining of the stomach and the first part of the gut known as the duodenum produce a natural mucous barrier. This protects the lining of the stomach and duodenum.
There is normally a balance between the amount of acid that you make and the mucous defence barrier. An ulcer may develop if there is an alteration in this balance, allowing the acid to damage the lining of the stomach or duodenum. Causes of this include the following:
Can Ulcers Cause Back Pain
Back pain is one among the less common symptoms of peptic ulcers. Here is a brief overview of ulcer symptoms that may include pain in the back.
Back pain is one among the less common symptoms of peptic ulcers. Here is a brief overview of ulcer symptoms that may include pain in the back.
Ulcers are very common in humans, especially middle-aged people. Peptic ulcers develop on the mucous membrane that lines the inner surfaces of the stomach and the duodenum. Esophageal ulcers form in the esophagus. Ulcers in the stomach are called gastric ulcers, and those in the duodenum are called duodenal ulcers. While duodenal ulcers are far more common than gastric ulcers, esophageal ulcers are rare. It has been observed that alcohol abuse is a major cause for ulcers in the esophagus. Peptic ulcers are usually associated with Helicobacter pylori infection or long-term use of NSAIDs. Ulcers can cause various symptoms, and abdominal pain is the most common one. Ulcers can also cause back pain, which is a symptom that is usually associated with other medical conditions.
Recommended Reading: How Common Is Ulcerative Colitis
Recommended Reading: What To Do About Upset Stomach And Diarrhea
Surgical Treatment Methods For Severe Diabetic Gastroparesis
In severe cases, the NIDDK says alternative food-delivery methods become inevitable to ensure youre getting adequate calories and nutrients. While the idea sounds overwhelming and scary, some of these options are far less invasive than others.
Feeding Tubes: Essentially, while sedated, a doctor will put a tube into your mouth or nose that extends all the way into your small intestine. Youll be placed on a liquid diet, and the feeding tube will allow those calories and nutrients to go directing into your small intestine, completely skipping the area with the most trouble: your stomach.
There are two types of feeding tubes to discuss with your healthcare team:
- a traditional oral or nasal feeding tube
- Jejunostomy feeding tube
Intravenous Nutrition:The last method of delivering adequate calories and nutrients without involving your stomach, is called Parenteral nutrition. Essentially, its a short-term intravenous solution that delivers liquid nutrients and calories directly into your bloodstream.
Venting Gastrostomy: This gadget is designed to relieve pressure inside your stomach by creating a very small opening on the side of your abdominal wall and then into your stomach. A tube is then placed through this opening, allowing stomach contents to flow out of the tube and into an external device that you attach to the tube when you need to relieve severe stomach pain.
Low Or High Blood Sugar
Low blood sugar occurs when your blood glucose drops below your target range. This usually happens at less than 70 mg/dl, but everyones range is different. It is best to talk to your healthcare provider about what is healthy for you. Often, when you experience low blood sugar, you will need to take action to fix it quickly.
Recommended Reading: How To Fix Severe Stomach Pain
What Is The Cause Of Peptic Ulcers
When you eat, your stomach produces hydrochloric acid and an enzyme called pepsin to digest the food.
- The food is partially digested in the stomach and then moves on to the duodenum to continue the process.
- Peptic ulcers occur when the acid and enzyme overcome the defense mechanisms of the gastrointestinal tract and erode the mucosal wall.
In the past it was thought that ulcers were caused by lifestyle factors such as eating habits, cigarettesmoking, and stress.
- Now it is understood that people with ulcers have an imbalance between acid and pepsin coupled with the digestive tractâs inability to protect itself from these harsh substances.
- Research done in the 1980s showed that some ulcers are caused by infection with a bacterium named Helicobacter pylori, usually called H pylori.
- Not everyone who gets an ulcer is infected with H pylori. Aspirin and nonsteroidal anti-inflammatory drugs can cause ulcers if taken regularly.
Some types of medical therapy can contribute to ulcer formation. The following factors can weaken the protective mucosal barrier of the stomach increasing the chances of getting an ulcer and slow the healing of existing ulcers.
- Aspirin, nonsteroidal anti-inflammatory drugs , and newer anti-inflammatory medications
- Cigarettesmoking
- Radiation therapy:-used for diseases such as cancer
People who take aspirin or other anti-inflammatory medications are at an increased risk even if they do not have H pylori infection.
When To Call The Doctor
See your healthcare provider if you have diabetes and you have:
- Frequent diarrhea.
- Other uncomfortable abdominal symptoms.
A note from Cleveland Clinic
All too often, diabetes and diarrhea go together. People with diabetes may experience frequent diarrhea loose, watery stools that happen at least three times a day. You may have fecal incontinence as well, especially at night. Diarrhea can also be due to metformin, a diabetes medication. If you have diarrhea, an upset stomach or constipation, talk to your healthcare provider. Medications and the right diet plan can relieve diarrhea, so you feel your best.
Last reviewed by a Cleveland Clinic medical professional on 04/25/2022.
References
Recommended Reading: How To Control Stomach Bloating
What Else Could The Patient Have
The differential diagnosis of GI complications of diabetes is very broad and includes other functional, motor, inflammatory, neoplastic, and endocrine disorders.
Diabetic Gastroparesis/Gastropathy
Patients with evidence of gastroparesis require screening for additional disorders including gastric outlet obstruction, thyroid dysfunction, neurologic disease, autoimmune disorders, prior gastric or bariatric surgery, and recent viral illness. In a tertiary care setting, the majority of gastroparesis cases are idiopathic , diabetic , or postsurgical .
As the name implies, idiopathic gastroparesis are those cases without a primary underlying etiology. Postsurgical gastroparesis is a consequence of intentional vagotomy or inadvertent vagus nerve injury. Other iatrogenic causes of gastroparesis are due to medications with anticholinergic properties, opiates for chronic pain , antidepressants in several classes , smoking cessation medications , and medications used for the treatment of diabetes .
Small Intestinal Bacterial Overgrowth
Table IV.
FODMAP Diet
Diabetic Constipation
Diabetic Diarrhea
Other conditions that cause diarrhea include inflammatory bowel disease, microscopic colitis, chronic intestinal infection with Giardia lamblia, rarer infections , other endocrinopathies , and intentional or unknowing ingestion of laxatives. As with SIBO, dietary factors should also be considered.
Fecal Incontinence
Miscellaneous GI Complications of Diabetes
How Are Peptic Ulcers Diagnosed
Your healthcare provider will look at your past health and give you a physical exam. You may also have some tests.
Imaging tests used to diagnose ulcers include:
- Upper GI series or barium swallow. This test looks at the organs of the top part of your digestive system. It checks your food pipe , stomach, and the first part of the small intestine . You will swallow a metallic fluid called barium. Barium coats the organs so that they can be seen on an X-ray.
- Upper endoscopy or EGD . This test looks at the lining of your esophagus, stomach, and duodenum. It uses a thin lighted tube called an endoscope. The tube has a camera at one end. The tube is put into your mouth and throat. Then it goes into your esophagus, stomach, and duodenum. Your health care provider can see the inside of these organs. A small tissue sample can be taken. This can be checked for H. pylori.
You may also have the following lab tests to see if you have an H. pylori infection:
Also Check: What Should You Eat When You Have Ulcerative Colitis
You May Like: Does Colon Cancer Cause Stomach Pain
When To Seek Medical Advice
See a GP if you’re experiencing symptoms of gastroparesis, as it can lead to some potentially serious complications.
These complications include:
- dehydration from repeated vomiting
- gastro-oesophageal reflux disease where stomach acid leaks out of your stomach and into your food pipe
- malnutrition when your body is not getting enough nutrients
- unpredictable blood sugar levels this is a particular risk in people with diabetes
What Exactly Is Diabetic Gut
Gastroparesis impairs the stomachs ability to transport food into the intestines, resulting in bloating, nausea, and heartburn. When diabetes is the culprit, clinicians refer to the disorder as diabetic gastroparesis. This page discusses the origins, symptoms, consequences, and therapies for diabetic gastroparesis.
Also Check: Why Is My Stomach Hurting For No Reason
Involvement Of Intestinal Control Pathways
Like the stomach, the activity of the intestine is determined by its content. The intestine manages its content by different types of annular contractions, which, depending on their temporo-spatial pattern, may produce segmentation/mixing or propulsion of contents. The organisation of intestinal contractile activity is still poorly understood. Diabetic neuropathy may disturb the regulation of intestinal motility and manifest as diverse symptoms such as diarrhoea, constipation, intestinal distension or abdominal pain . These symptoms may present simultaneously or may alternate over time.
What Tests Diagnose A Peptic Ulcer
To confirm a person has an ulcer a diagnostic imaging test will usually be ordered. The two most widely used tests are:
- Upper GI series : This is a type of X-ray. The patient is given a chalky liquid to drink that increases the contrast on the X-ray, making certain features easier to see. Because this liquid contains barium, this test is sometimes called a barium swallow.
- Endoscopy : An endoscope is a thin, flexible tube with a tiny camera at the end. The patient is given a mild sedative, and then the tube is passed through the mouth into the stomach. The doctor can see the lining of the stomach to diagnose a peptic ulcer. Tiny samples of the tissue will be taken , which are examined under a microscope.
If a diagnostic imaging test reveals an ulcer, the patient will most likely have a test to see if H pylori bacteria are present.
- It is important to be certain about this, because treatment of the H pylori is likely to heal the ulcer.
- Ulcers caused by H pylori are treated differently than ulcers caused by medications.
Three types of tests are available to detect H pylori.
Recommended Reading: Why Do I Keep Having Stomach Pains
Go For Water Instead Of Sugary Beverages
Drinking water as your primary beverage will help you avoid sugary drinks, which increase complications of gastroparesis. On the one hand, sweetened fruit juice and sugary sodas have increased the risk of type 2 diabetes in adults. On the other hand, increased water intake results in better insulin response and blood sugar control.
Reports suggest that taking an extra half serving of sugary drinks can increase the risk of type 2 diabetes by 18%, translating into an increased risk of gastroparesis. On the flip side, 24-week research of overweight adult women shows that using water to replace diet soda in a weight loss program will help reduce your insulin resistance.
Summarily, drinking water helps eliminate excess blood sugar otherwise triggered by sugary beverages.
When To Seek Emergency Care
Nausea and vomiting can be also be indicators of more serious health issues. Seek emergency care if your nausea and vomiting persist four more than a few hours, result bloody or odd-colored vomit or discharge. or is accompanied by high fever, stiff neck, hallucinations, chest pain, or severe abdominal pain with no explanation.
Recommended Reading: How To Make Your Stomach Smaller
Stomach Pain In Diabetics: Causes And Treatments
Many stomach aches result from temporary gastrointestinal issues which are soon resolved. However, stomach pain may be a sign of a more serious problem such as diabetic gastroparesis which is a result of delayed bowel movement. This inability of the stomach to empty normally leads to a stomach ache referred to as diabetes stomach pain. The condition usually occurs in individuals with diabetes type 1 although it can also affect those with type 2 diabetes. But what are the characteristics of gastroparesis and how is it treated?
Celiac Disease And Type 1 Diabetes
While it is unclear exactly what the relationship is, some research has found that those with celiac disease are more likely than the general population to develop type 1 diabetes. One 2015 study found that type 1 diabetes affected only 0.4% of the control subjects, but 3.2% of those with celiac disease.7
You May Like: What’s The Best Workout For Stomach Fat
Are You Sure The Patient Has A Gastrointestinal Complication Of Diabetes
Diabetes is associated with a range of complications involving the gastrointestinal tract, biliary tree, pancreas, and liver . Up to 75% of patients with longstanding diabetes report chronic or intermittent GI complaints resulting from abnormal sensory or motor function of the gut. Patient with diabetes may have altered function of multiple organs as evidenced in studies using methods to assess transit or motor function in several gut regions .
Table I.
Diabetes and GI Diseases
Diabetic Gastroparesis/Gastropathy
Definition: Diabetic gastropathy is a term used to collectively describe all disorders that occur as a result of autonomic neuropathy affecting the stomach. The most severe disorder is gastroparesis which is defined by delayed gastric emptying in the absence of mechanical obstruction. Approximately 40% of patients with type 1 diabetes and 10-20% of patients with type 2 diabetes will develop gastroparesis.
An expert consensus group has proposed the following grading system for gastroparesis:
Grade 1symptoms controlled with maintenance of weight and nutrition on a standard diet
Grade 2moderate symptoms with partial control on prokinetic and antiemetic medications and ability to maintain nutrition with dietary modifications
Grade 3refractory, uncontrolled symptoms requiring frequent emergency department and clinic visits or hospitalizations and/or inability to maintain nutrition orally
Table II.
Gastroparesis Cardinal Symptom Index
Diabetic Constipation
Table III.
What Is The Diabetic Stomach
Diabetes-related abdominal obesity is a major issue that may possibly indicate heart failure. Many individuals are unaware that the stubborn fat around the waist, which is difficult to eliminate, is caused by an insulin deficiency. If you have excessive blood sugar, there is a strong likelihood that you have difficulty eliminating waist fat.
Also Check: What Do You Take For Stomach Flu
Risk Factors And Prevalence
Gastroparesis is a common complication of diabetes. About 20%50% of people with diabetes will experience diabetic gastroparesis. Gastroparesis is more common in people who have type 1 diabetes and in those who have had type 2 diabetes for more than 10 years.
Having poor control of blood sugar, retinopathy , or neuropathy are risk factors associated with increased rates of diabetic gastroparesis.
Being female, smoking, and having obesity can also raise the risk for gastroparesis.
Lauras Advice To Other Patients Struggling With Gastroparesis
First and foremost, Laura says its crucial to make sure youre researching the condition yourself , and make sure youre using credible sources when learning about potential treatments.
I found that I had to accept that many healthcare professionals did not have a great understanding about the condition however, I do appreciate their honesty in telling me this. And we have worked together to manage it as best we can.
Laura absolutely recommends joining social media forums or support groups to talk to others about their own methods of managing the grueling symptoms of gastroparesis.
The patients really are the experts, and they have many tricks up their sleeves to make living with this difficult condition more manageable.
If you found this guide to diabetic gastroparesis helpful, please sign up for our newsletter in the form below. We send out a weekly newsletter with the latest posts and recipes from Diabetes Strong.
You May Like: How Do I Flatten My Upper Stomach